Best Deals for all new
Best Gifts For Cancer Women
Find the best product for your choice that you can comfortably use in 2023 and beyond

Featured Items
Added to wishlistRemoved from wishlist 0

Lung Cancer Whisperer Survivor Gifts – Travel Mug Insulated Coffee Tumbler – Lung Cancer Awareness Malignant Tumor Warrior Chemo Patient Themed
$21.95
Added to wishlistRemoved from wishlist 0

Thyroid Cancer Survivor AF Gifts – Travel Mug Insulated Coffee Tumbler – Malignant Thyroid Gland Cancer Awareness Warrior Chemo Patient Themed
$21.95
Added to wishlistRemoved from wishlist 0

Non-Hodgkin’s Lymphoma Warrior Themed – Travel Mug Insulated Coffee Tumbler – Non-Hodgkin Lymphatic Cancer Tumor Awareness Warrior Chemo Survivor Patient Gifts
$21.95
Added to wishlistRemoved from wishlist 0

Prostate Cancer Warrior Gifts – Travel Mug Insulated Coffee Tumbler – Mens Prostate Malignant Tumor Chemo PSA Survivor Cancer Patient Awareness Themed
$21.95
Added to wishlistRemoved from wishlist 0

Pancreatic Cancer Survivor Awareness Gifts – Travel Mug Insulated Coffee Tumbler – Pancreas Malignant Tumor Cancer Warrior Chemo Patient Themed
$21.95
Added to wishlistRemoved from wishlist 0

Testicular Cancer Survivor Themed Gifts – Travel Mug Insulated Coffee Tumbler – Malignant Testicle Cancer Awareness Warrior Chemo Patient Men – Straight Outta Testicular Cancer
$21.95
Added to wishlistRemoved from wishlist 0

Pancreatic Cancer Survivor Awareness Gifts – Travel Mug Insulated Coffee Tumbler – Pancreas Malignant Tumor Cancer Warrior Chemo Patient Themed – Beat Got This Mug
$21.95
Added to wishlistRemoved from wishlist 0

Badass Testicular Cancer Survivor Themed Gifts – Travel Mug Insulated Coffee Tumbler – Malignant Testicle Cancer Awareness Warrior Chemo Patient Men – This Mug Belongs
$21.95
Added to wishlistRemoved from wishlist 0

Liver Cancer Awareness Themed Gifts – Travel Mug Insulated Coffee Tumbler – Hepatocellular Carcinoma Cancer Malignant Tumor Warrior Chemo Survivor Patient – This Mug Belongs Warrior
$21.95
Added to wishlistRemoved from wishlist 0

I Beat Cancer Survivor Travel Mug Insulated Coffee Tumbler – Chemotherapy Warrior Chemo Cancer Patient Awareness Motivational Inspirational Care Package Funny Cute Gifts Idea
$21.95
Added to wishlistRemoved from wishlist 0

Im a Bladder Cancer Survivor and Awesome Travel Mug Insulated Coffee Tumbler – Bladder Cancer Warrior Chemo Patient Awareness Care Package Motivational Themed Gifts
$21.95
Added to wishlistRemoved from wishlist 0

Im a Bladder Cancer Survivor Bitches Travel Mug Insulated Coffee Tumbler – Bladder Cancer Warrior Chemo Patient Awareness Care Package Motivational Themed Gifts
$21.95
Choose category

Latest Products
- Show all
- Popular
- Best rated
- Choose category
- All categories
- Dammit Dolls
- Bags
- Cancer Books
- Candles
- Clothes
- Comfort Caring Items
- Games
- Gift Sets
- Hair Care
- Headphones
- Jewelry
- Mugs
- Shoes
- Skin Care
- Smartwatches
- Toothbrush
Added to wishlistRemoved from wishlist 0
$19.99
Knit Scarf/Hat/Gloves Set, Soft Warm Beanie, Touch Screen Unisex Cable Knit Winter Cold Weather Gift
Added to wishlistRemoved from wishlist 0
$22.98
Added to wishlistRemoved from wishlist 0
$4.99
Added to wishlistRemoved from wishlist 0
$11.99
Added to wishlistRemoved from wishlist 0
$19.99
Added to wishlistRemoved from wishlist 0
$24.99
Added to wishlistRemoved from wishlist 0
$7.00
Added to wishlistRemoved from wishlist 0
$32.99
Added to wishlistRemoved from wishlist 0
$13.95
Added to wishlistRemoved from wishlist 0
25%
Top Selling Products
Save a lot of money and time, get best deals
Added to wishlistRemoved from wishlist 0

Be Brave Quote Necklace Gift for Sick Woman Patient Friend Encouragement Uplifting Motivation Recovery Gift Idea Fighting Cancer
$37.99
Added to wishlistRemoved from wishlist 0

Pancreatic Awareness Gift Pancreatic Purple Ribbon Necklace Pancreatic Cancer Support Jewelry
$12.86
Added to wishlistRemoved from wishlist 0

F A Dumont Sterling Silver St. Giles Pendant with 18" Stainless Steel Lite Curb Chain. Patron Saint of Cancer Patients
$51.50
Added to wishlistRemoved from wishlist 0

HOLLP Breast Cancer Survivor Gift Cancer Awareness Necklace Pink Ribbon Rhinestone Necklace Cancer Survivor Fighter Jewelry Inspirational Gift for Women
$14.68
Added to wishlistRemoved from wishlist 0

Customized Necklace You Aren T Alone Cancer Patient Necklace Inspirational Gift For Cancer Patient Love Knot Necklace Message Card Gift Box Jewelry Heart Diamond Charm Pendant For Anniversary
$44.95
Added to wishlistRemoved from wishlist 0

Sterling Silver St. Peregrine with 18 in. Rhodium Plated Brass Chain and Deluxe Gift Box – Cancer Patients
$49.99
Added to wishlistRemoved from wishlist 0

My Very Best Horoscope Constellation Zodiac Sign Necklace
$8.99
Added to wishlistRemoved from wishlist 0

Personalized Jewelry Gift – Inspirational Necklace Gift, Necklace for Patient Warrior, Gift for Cancer Patient, Be Strong Necklace, Fighter Gift, Forever Love. wedding day gift, gift for bride
$35.99
Added to wishlistRemoved from wishlist 0

The Love Knot Necklace You aren’t alone Cancer Support Gift, Support Gift for Cancer patient, Uplifting Gift for friend, Thinking of You Gift Cancer Survivor Gift Unique Gift Necklace for Birthday
$32.59
Added to wishlistRemoved from wishlist 0

MAOFAED Warrior Gift Survivor Gift Cancer Fighter Gift You Are Stronger Thank You Think Morse Code Necklace
$15.89
Added to wishlistRemoved from wishlist 0

Muse Infinite Don’t Quit Quote AA Gift Uplift Sick Friend Get Well Soon Gift for Woman Cancer Patient Don’t Lose Hope Gift Idea
$39.99
Added to wishlistRemoved from wishlist 0
Message Card Jewelry, Handmade Necklace- Personalized Gift Cancer Survivor Gift, Breast for Patient, Surgery Gifts, Awareness Girl Boss Chemo Custom Size
$34.99
Added to wishlistRemoved from wishlist 0

Get Better Gift for Woman Patient Cancer Survivor Necklace Get Well Gift Sick Friend Get Well Soon Motivation Encouragement
$39.99
Added to wishlistRemoved from wishlist 0

St. Peregrine, Patron of Cancer Patients and Those Cured of Cancer: Handmade Medal
$22.95
Added to wishlistRemoved from wishlist 0

Patron Saint of Cancer Locket Necklace, St. Peregrine, Cancer Patient Get Well Gift, Encouragement, Hope
$42.00
Added to wishlistRemoved from wishlist 0

Fighter Quote Gift for Woman, Courage Necklace for Sick Friend, Woman Patient Cancer Survivor Fighting Illness Recovery
$37.99
Added to wishlistRemoved from wishlist 0

LMXXV Free Engraving-Quality Stainless Steel Medical Alert ID Dog Tag Pendant Necklace for Men Women,24″/26″/28″
$9.99
Added to wishlistRemoved from wishlist 0

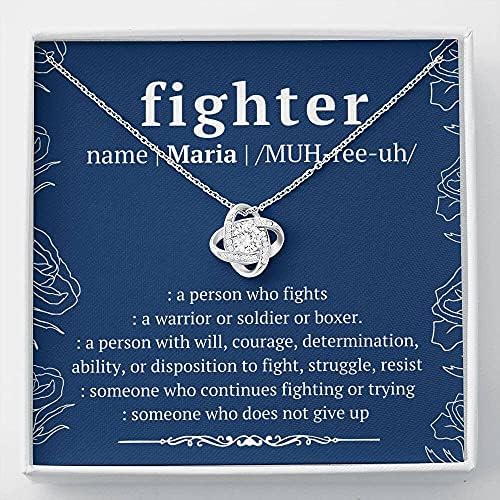
KUIYAI Cancer Support Gift Cancer Survivor Gift Fighter Warrior Gift Sick Friend Gift Inspirational Gift For Cancer Patient
$11.99
Added to wishlistRemoved from wishlist 0

Message Jewelry – Cancer Survivor Gift For Cancer Patient, After Chemo Mastectomy, Cancer Fighter Necklace, Breast Cancer Survivor Gift With Necklaces styles On Birthday, Xmas with Message Card & Box
$34.99
Added to wishlistRemoved from wishlist 0

Spinningdaisy Breast Cancer Awareness Sleek Pink Ribbon Necklace
$11.99
Added to wishlistRemoved from wishlist 0

Leukemia Warrior Necklace – Gift for Support, Fighter, Survivor – Orange Ribbon Awareness – Jewelry for Post-Surgery, Chemo Patient
$44.99
Added to wishlistRemoved from wishlist 0

Strength Necklace • Addiction Recovery • Survivor Gift • Silver Necklace • Strength • Encouragement • Cancer Divorce Single Mom Depression • Inspirational Gifts (Infinity Heart)
$49.95
Added to wishlistRemoved from wishlist 0

YFN Inspirational Necklace Sterling Silver Graduation Pendant Jewelry Graduation Gifts for Women Men Girls Boys
$32.99
Added to wishlistRemoved from wishlist 0

18-Inch Rhodium Plated Necklace with 4mm Jet Birthstone Beads and Saint Giles Charm. Patron Saint of Cancer Patients
$81.00
Added to wishlistRemoved from wishlist 0

Message Card Jewelry – Gifts for Women, Handmade Necklace Personalized You Are Not Alone, Cancer Support Necklace, Surgery, Cancer Patient, Sick Friend Gift, Care Package, You’re Not Alone
$29.99
Added to wishlistRemoved from wishlist 0

Cancer Patient – Necklace – Tag-Z Dog Tags
$9.00
Added to wishlistRemoved from wishlist 0

Appendix Cancer Warrior Necklace – Gift for Support, Fighter, Survivor – Amber Ribbon Awareness – Jewelry for Post-Surgery, Chemo Patient
$44.99
Added to wishlistRemoved from wishlist 0

Zealmer Retro 12 Zodiac Old English Letter Necklace for Women
$14.98
Added to wishlistRemoved from wishlist 0

Message Card Jewelry, Handmade Necklace- Personalized Gift Cancer Patient Jewelry, Personalized Warrior Necklace, Cancer Survivor Custom Gift for Women, You are a Warrior Card, Strength Keepsake AC11
$34.99
Added to wishlistRemoved from wishlist 0

Pre-Engraved & Customizable Cancer Patient Alert Medical ID Necklace – 22in/56cm
$28.79















